KG Jebsen Coeliac Disease Research Centre, Norway
For our second ‘meet the researchers’ feature we bring you the KG Jebsen Coeliac Disease Research Centre (JCoDiRC) Oslo, Norway. Professor Ludvig Sollid leads this super talented team of scientists. You will also notice throughout the introductions that there is an artist among them who has explained difficult science, in a series of cartoons.
 Meet the researchers:
Meet the researchers:
- Ludvig Sollid – Medical Doctor, Immunologist and Director of the KG Jebsen Coeliac Disease Research Centre
- Asbjørn Christophersen and Louise Fremgaard Risnes – Postdoc researchers
- Rasmus Iversen - Researcher, Lene Høydahl - Postdoc researcher and Ida Lindeman - PhD student
- Shuo-Wang Qiao - Associate Professor of Immunology, Shiva Dahal-Koirala - Postdoc researcher and Geir-Kjetil Sandve - Associate Professor of Informatics
- Knut Lundin - Clinical Gastroenterologist, Stephanie Zühlke - PhD student and Jorunn Stamnæs - Researcher
All cartoons credited to Jorunn Stamnæs, JCoDiRC, Norway
At the end of the week, the talented researchers at JCoDiRC took part in an online Q&A over on our Facebook page answering questions from our gluten free community on coeliac disease, their current research and the researchers themselves.
Take a look at the Frequently Asked Questions below to see their response.
Frequently Asked Questions
Last I heard the 'injection trial' as a cure for coeliac disease was stopped as there was no significant evidence that it would be helpful. Has that research started again or is there now a new set of research? What is the research focusing on now?
I assume you are thinking about the clinical trial of ImmusanT that had the goal to re-educate gluten-reactive T cells. Yes, you are right this trial was stopped last summer after an interim analysis as it became clear that the drug was not effective.
Such setbacks are not unusual in drug development. In fact, it is considered that only one out of ten candidate drugs become a real drug for treatment of patients.
There are many other drugs for coeliac disease in the pipeline. Hopefully, one or more of these will make it so that a non-dietary treatment alternative becomes a reality for coeliac disease.
It seems as though there are types of coeliac disease (in the same way we are reclassifying types of diabetes) for example 'silent coeliacs' have fewer acute GI issues. Is this likely to lead to a reclassification of disease types and can you imagine differing treatments which can limit the absorption of gluten to the extent that those with fewer acute GI upset may be able to tolerate lower levels of gluten in the future?
Actually, not much is known as to why some people react more strongly to gluten exposure than others, but the amount of signal substances from T cells correlates with the degree of severity of symptoms. It is not very likely that this release of signal substances from T cells correlates with other consequences of coeliac disease.
Is there much research into dental/oral problems in people with coeliac disease, and if not can we do some? I work in dental research and would love to link my work and my diet.
No, not much research now. We suspect the dental problems in coeliac disease are under-reported. There used to be some dentists working with clinical studies on this.
Is there currently any research into Refractory coeliac disease I and II? Just been diagnosed with refractory 1 and it seems very little is known about it?
Yes, there is research on both, in particular refractory coeliac disease II with malignant cells.
Basic science studies and a very few drug trials have been done or are ongoing. refractory coeliac disease I is tricky. It is for sure a mixed bag where inadvertent, continuous gluten exposure is a frequent cause.
In many other cases, the patient is clinically well, but the gut takes a long time to heal.
What can cause continuous villous blunting and increase in lymphocytes despite following a strict gluten free diet and caution against cross contamination? I have also had investigations for other IBD and nothing was seen.
For some patients, recovery to a normal mucosa (no villous blunting) can take several years on a gluten free diet. A few patients also fail to recover despite a strict gluten free diet. We do not really know yet why this is, but in most cases very small amounts of gluten are the cause, as some patients respond stronger to small amounts of gluten than others. However, clinical symptoms may still disappear despite the presence of villous blunting.
How close are we to understanding what causes coeliac disease, particularly why some people with the genes do not go on to develop it? And how helpful is this line of research to us? Will it lead to developing preventative measures?
Our current understanding of the disease mechanism in coeliac disease is way better than for other immune mediated diseases like type 1 diabetes or rheumatoid arthritis. Yet, there is still a lot we do not understand. For instance, as you mention, why not everybody who carries the genes for HLA-DQ2 or HLA-DQ8 does not develop the disease. We know that genes other than the HLA genes are implicated in the development of coeliac disease.
Many people who carry the HLA-DQ2/DQ8 do not develop coeliac disease and so it’s most likely they lack some of these other non-HLA susceptibility genes. In addition, we strongly believe that environmental factors other than gluten, for instance diarrheal viruses, are involved in coeliac disease development.
Some HLA-DQ2/DQ8 carriers who do not develop coeliac disease may have avoided a critical viral infection.
There is much to learn. The ultimate goal, and what hopefully can be achieved with even better insight, is prevention of coeliac disease.
Have they come up with a magic cure yet so we can eat anything?
No, not yet.
No drugs are accepted as non-dietary treatment. We all have hopes that such drugs will come to the market. They may be used for accidental exposure, and maybe as a cure.
If their research is successful and the blood test comes to fruition that would help so many who are in no man’s land of diagnosis since they either weren’t or couldn’t have sufficient gluten containing food for the other bloods and biopsies. When would this test be available?
For the HLA-DQ:gluten tetramer test to become available in clinical practise, production of the test must be industrialised (that means, manufactured for sale).
This process is ongoing and will hopefully be successful. In addition, the test must be validated for its performance when samples are sent in from many patients from different doctors to the analysing laboratories. All this will take some time, maybe a year or two if everything goes well.
Please can you explain the T cells as I keep getting gut spasms?
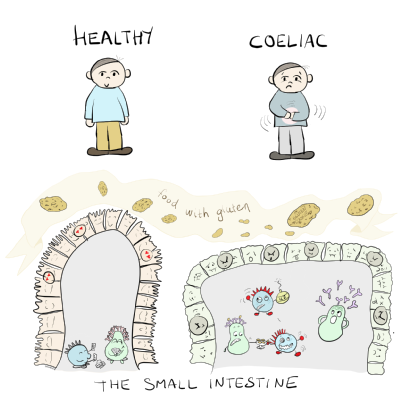
T cells are special cells that are part of our immune system. They protect us against pathogens.
In individuals with coeliac disease, some of these T cells will go crazy when they meet gluten. This causes inflammation in the intestine when you eat gluten. The diagnosis of coeliac disease is relatively easy to achieve compared to many other gastrointestinal disorders, and all of those tests should be available from your local GP.
Is it considered normal for ttg levels to drop dramatically in one year, or is this considered an erroneous result? (I.e. On the scale where 10> is positive, dropping from a ttg level in the 100s down to <4 in one year)
Yes, such a drop can often be seen when the patient is fully compliant with a gluten free diet.
How common is thrombocytopenia in coeliac disease and how should it be managed?
I think it is quite infrequent. But some patients have several immune disorders at the same time, unfortunately.
Why does the body have transglutaminase, can you live without it – get rid of it? If so, would this cure Coeliac Disease?
Transglutaminase 2 (TG2) is a wound healing enzyme, and its natural role is to crosslink proteins in the body. We cannot remove TG2 but we can inhibit the enzymatic activity of TG2. This would prevent TG2 from modifying gluten peptides in the gut. Because the T cells that respond to gluten in coeliac disease depend on this modification, we think that inhibition of TG2 activity should prevent the activation of gluten specific T cells.
A drug that does exactly that, a TG2 inhibitor, is currently tested in patients with coeliac disease (clinical trial by Dr. Falk Pharma). This is a good example of observations from the clinic (antibodies to TG2, and gluten specific T cells from gut biopsies) that were studied in the lab and where the discovered mechanisms have led to development of therapy.
Question to Ludvig Sollid – why did you choose to research coeliac disease and stay interested in it?
By chance as many other things in life.
I was a medical student and wanted to do research. In the medical school curriculum, cellular immunology had fascinated me. I thus contacted immunology professor Per Brandtzaeg to ask whether there was an option to take a gap year and get involved in research. Per had just supervised a doctor (Helge Scott) together with another immunology professor Erik Thorsby. The PhD thesis of Helge was on the topic of immunology of coeliac disease. Per and Erik suggested I should follow the paths of Helge as this would also include studies of T cells. I thought this was a good suggestion and started.
After several backlashes and a feeling of being completely useless, I made progress. I took another leave from medical school and during this period I made the discovery of HLA-DQ2 being a culprit molecule in coeliac disease. I was utterly fascinated and absorbed by science and after medical school and completing service to become a licensed doctor, I went back to the lab. I have more or less worked there since.
Do you know if clinical trials for coeliac disease will come to the UK?
This is what is listed on ClinicalTrials at the moment.
Professor Sanders in Sheffield took part in the gluten degrading enzyme trial sponsored by Alvine Pharmaceuticals. There are no UK centres in the ongoing (recruitment completed) trial with transglutaminase 2 inhibitor by Dr. Falk Pharma.
The UK should be a good place to do studies, and there are several trials coming.
Will Stephanie’s research result in a blood test to see if you are sticking to your gluten free diet?
Yes, we hope so.
Stephanie has looked at certain markers on the gluten specific T cells and how quickly they appear in response to gluten. If we include this marker with the HLA-DQ:gluten tetramer test, we may be able to say something about whether patients have eaten gluten recently or not. We need to perform further validation of this phenomenon before we can use it in a clinical setting.
Will Jorunn’s research looking at the proteins be able to tell you if someone has coeliac disease or refractory coeliac disease?
Not yet, but we hope that such distinctions can be made in the future.
At the moment it is not clear whether refractory coeliac disease (RCD) type I is mechanistically similar to or different from untreated coleiac disease, even though we know that RCD I patients have little or no effect of a gluten free diet. We have not yet studied RCD samples by our protein analysis approach, but we plan to do so in near future.
How successful was the Celimmune trial for refractory coeliac disease? What did it involve?
The study was published last year.
The primary endpoint was not met, unfortunately, but some effect was seen. Some patients benefitted from the treatment, but their problems were not solved overall. The drug may be developed further, but many of us were a bit disappointed by the result.
Why do the T cells respond to gluten in wheat, barley and rye? Why do some respond to the gluten in oats?
The short answer is that we believe it is more difficult to make immune (T-cell) responses to gluten proteins of oats than to gluten proteins of the other cereals.
Coeliacs have T cells responding to certain peptides (what immunologists call epitopes) of wheat, barley and rye. (BTW: all peptides have to be modified by transglutaminase 2 in the body before T cells will recognise them). Some epitopes are shared between different grain types, some are specific for a certain type of grain. What initiates the response to a given epitope and the expansion of specific T cell clones that follows, we believe is related to how much of an epitope will survive gut digestion. After an initial sensitisation to an epitope, the immune system becomes very sensitive to this epitope requiring very little to get fired up. The epitopes of oats that some very few coeliacs mount responses to, are part of cereal proteins that are not very resistant to digestion by the gut digestive enzymes. This is in contrast to most other gluten epitopes of wheat, barley and rye. Thus, it is less of a chance to get sensitised to oats.
If you remove the gluten specific T cells, will other T cells just change and take their place?
The biggest question is whether the treatment with removal of gluten-specific T cells will be sufficiently effective.
It is possible that if a few gluten-reactive T cells remain. These cells can expand on a new contact with gluten - and then the problem is back. It is also possible that there will be sensitisation of naive T cells that have not seen gluten before.
Basically, the initiation of coeliac disease from the beginning might again happen. This latter scenario we consider to be less of a problem though.
I would like to ask if coeliac disease makes Corona virus more deadly....I have been told to have flu vaccine and pneumococcal as chances are my spleen doesn't work properly to protect me.
Individuals with coeliac disease are not considered at higher risk of catching the flu or other viral or bacterial infectious diseases than non-coeliac individuals unless they have hyposplenism (a small spleen with reduced function). There is an increased risk of hyposlenism in people with coeliac disease compared with the general population, but risk is small.
Why hyposplenism develops in some people, we do not know. Coeliac disease in the absence of hyposplenism does not affect the overall immune system. In the disease process driven by gluten exposure, only a small fraction of all your immune cells get involved. While this immune response makes it very uncomfortable to eat gluten, it is unlikely to have an overall effect on the immune system unless the person has hyposplenisms. As it is unlikely to be tested for hyposplenism, people with coeliac disease are recommended to take certain vaccines.
I’ve heard lots about cures. Enzymes that they use in beers to break down gluten: making them gluten free. Might this be a possible thing used in tablet form? How far are we off something more significant than the gluten free diet?
Actually the same enzyme is already on the market as Tolerase G in the US and with other trade names in Europe. It works during brewing of beer and also in human stomachs, but has not been tested properly as a treatment in coeliac disease. And it probably won’t work if for instance you drink milk with the enzyme.
Will the pill from Dr Falk replace the gluten free diet or will it help with the gluten free diet?
Probably, the ambition is this treatment will replace the gluten free diet (but this will be for the company to decide).
Why was the Alvine Pharmaceutical trial unsuccessful?
This trial was unsuccessful due to what is called a trial effect. All the participants in this trial whether they received the drug or placebo (the dummy drug) got better so it was impossible to conclude whether the drug was effective or not.
If you remove the gluten specific T cells what effect will this have on the overall immune system?
We do not expect that this should have any effect on the immune system in general as the gluten specific T cells are only a small population in the total T cell population. Therefore it should be completely safe to remove the gluten specific T cells if we can target them specifically.
Is there a link between coeliac and addisons diseases. Should those with coeliac disease be tested for Addison’s as routine?
Addison’s disease also has an HLA association with the DR3-DQ2 and DR4-DQ8 haplotypes (some of the genes that predispose people to developing coeliac disease also predispose to Addison’s disease). Addison’s disease is a rare disorder so screening all people with coeliac disease for Addison’s disease would probably not be advised.
Are you doing any research on gluten related neurological conditions?
The short answer is no. The Sheffield group is doing very nice studies in the UK - very difficult to compete with them!
Are T cells also involved in Dermatitis Herpetiformis?
Yes, probably but not yet proven. It has not been well studied so far. Our centre is entering this field, but mainly on the B cell side.
Are the HLA molecules in coeliac disease involved in any other conditions?
Yes, they are. The genes encoding for DQ2 are involved in many autoimmune diseases (type 1 diabetes, Graves’ disease, Myasthenia gravis, Addison’s disease etc) and the genes encoding for DQ8 are involved in some diseases, for instance type 1 diabetes. In coeliac disease these HLA molecules present gluten peptides to T cells. In the other diseases we do not know which peptides they are presenting, but it is very unlikely that they are gluten derived peptides.
I’ve been on a gluten free diet for over 5 years but at my annual review my GP said my antibody blood test was positive. Is there anything other than having gluten in my diet that could cause a positive blood test?
Well, it depends a bit on which antibody test you refer to. The most frequently used is IgA against transglutaminase 2 (TG2). If that has been negative and now is positive, it indicates you are exposed to gluten. Are you well clinically? Have you had a repeat biopsy?
Does anyone in the research team have coeliac disease themselves?
Not at the moment, but we are several individuals with the DQ2 or DQ8 HLA types and several of us have close relatives with coeliac disease.
My 6 year old son has been diagnosed for 3 years and despite being on a strict gluten free diet and our home is completely gluten free his ttg levels remain high at 128. His paediatrician and dietician aren’t concerned as he is thriving and non symptomatic compared to pre diagnosis, where he was vomiting daily, dramatic loss of weight, fatigue etc. Should I be concerned as to why it isn’t coming down quickly?
This is a hard one to reply to as an adult gastroenterologist.
It is very good your son is doing better. I (Knut Lundin) have had that question several times and actually it seems that some people have persistent antibody levels. Why that happens and what to do about it is uncertain. In some cases it does turn out to be ongoing exposure to gluten. A test for gluten peptides in urine and faeces has been developed, but is not yet widely used, mainly in research.
We are exploring these tests in our Coeliac clinic and we do have some people with a positive test indicating exposure to gluten, although they consider themselves to be adhering to a strict gluten free diet.
Does everyone with potential coeliac disease go on to develop full blown coeliac disease or will someone stop producing antibodies and feel better?
No, probably not every potential coeliac will go on to develop the 'full-blown' disease. An issue here will be how long the individuals are followed up.
We also have evidence from studies of children that some who are positive for IgA anti-transglutaminase 2 antibodies in the blood, become negative for these antibodies. In these children we believe that they are on the way to develop disease, but then the disease process for some reason reverts. Whether the same can be the case in adults, it is not known. If so, it is probably not very common.